15 Million California Medi-Cal Enrollees to have Eligibility Status Reviewed
Starting this Month –Watch for Medi-Cal Notices in Your Mail
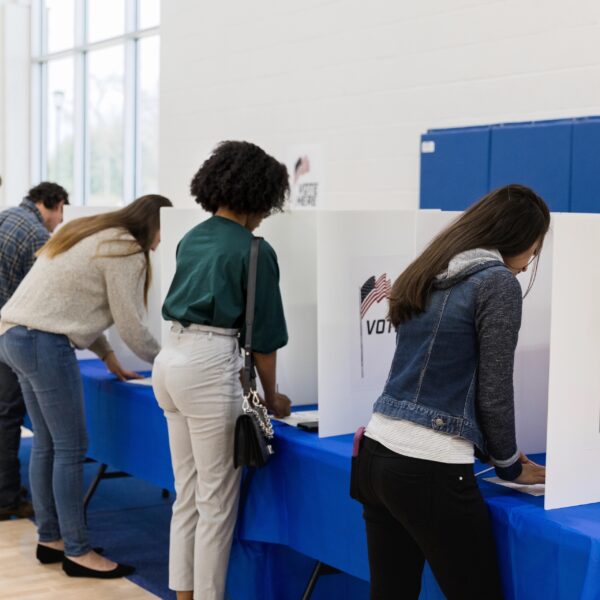
The special briefing sponsored by the California Department of Healthcare Services and organized by Ethnic Media Services and California black media, moderated by Sunita Sorabji EMS’s Healthcare Editor, provided crucial information about the redetermination process for the 15 million Medi-Cal enrollees in California. The briefing highlighted that after suspending the process throughout the Covid-19 pandemic, California now has 14 months to review the eligibility of these enrollees, during which an estimated two to three million Californians may leave the program nationwide, which is referred to as the “unwinding period.”
The briefing emphasized the importance for enrollees to be vigilant and watch out for notifications from their local Medi-Cal offices. Envelopes with yellow color indicate that more information is needed, and enrollees must respond promptly to maintain their coverage. Failure to respond or administrative barriers, such as outdated contact information at local Medi-Cal offices, could lead to dis-enrollment, putting enrollees at risk of losing their coverage.
Speakers at the briefing, including Yingjia Huang, Assistant Deputy Director from the Department of Health Care Services, and Mayra Alvarez, Executive Director of Children’s Partnership, provided insights into the redetermination process, discussed who may be at risk of dis-enrollment, and shared steps that enrollees can take to be prepared. The briefing also highlighted that information about the process is available in 19 languages on the DHCS website, including the availability of Maria Romero Mora from DHCS to respond to questions from attendees.
Overall, the briefing provided important information about the redetermination process for Medi-Cal enrollees in California emphasized the need for timely response to notifications, and highlighted resources available in multiple languages for enrollees to stay informed. It serves as a valuable resource for Californians who rely on Medi-Cal for their healthcare coverage.
Yingjia Huang, Assistant Deputy Director of the Department of Health Care Services provided an overview of the Medicaid renewal process for over 15 million individuals across the state of California during a briefing. The renewal process, which began on April 1st, had been delayed for three years due to federal rules related to the COVID-19 pandemic. Huang emphasized the importance of medical beneficiaries updating their contact information, including addresses, phone numbers, and emails, with their local medical County offices. This can be done online through County portals such as Benefits Cal or My Benefits Cal, where medical members can also check their renewal month and update their information. Huang mentioned that renewal dates will be different for each medical member and will occur between April 2023 and May 2024, lasting for 14 months. Medical members who are not automatically renewed will receive a packet in the mail in a yellow envelope, which can be completed online or by phone. It is critical for medical members to complete the renewal process by the due date to avoid coverage gaps. Huang also mentioned that if medical members are not eligible for medical, their information will be automatically sent to Covered California, the state’s exchange for purchasing insurance with a premium tax credit. The department is also working on eligibility expansions, including the 26 through 49 expansions and the elimination of assets, which will take effect on January 1st, 2024. Huang encouraged medical members to stay updated through the Department of Healthcare Services’ website and local medical offices.
Overall, the briefing provides important information about the Medicaid renewal process in California, including the need for medical members to update their contact information and complete the renewal process by the due date. The inclusion of online options for updating information and completing renewals is helpful, and the mention of upcoming eligibility expansions provides additional context. The briefing could be further improved by providing more details on how medical members can access the County portals and other resources, as well as emphasizing the consequences of not completing the renewal process by the due date, such as potential loss of coverage.
Mayra Alvarez, Executive Director of Children’s Partnership, is a strong advocate for child health equity and focuses on advancing the well-being of marginalized children in partnership with local and state partners. She emphasizes the importance of health insurance coverage and access to care, especially during the pandemic, which has exacerbated mental health issues for children and youth in California. Alvarez highlights that over half of all kids in California, including almost 70% of children of color, depend on medical coverage, which is a lifeline for many in the community.
Alvarez acknowledges that long-standing structurally racist policies and practices have created an environment where families of color experience greater degrees of instability in employment, income, and housing, leading to disruptions in health coverage. She provides examples of how even small errors or changes in addresses or jobs can result in procedural terminations and loss of coverage. She also mentions that burdensome administrative requests and barriers further risk disrupting coverage, leading to unnecessary loss of coverage for families and children who are still eligible.
Alvarez applauds the efforts to remove administrative hurdles and implement continuous coverage protections, which have helped millions of Californians stay covered. She urges for necessary steps to be taken to ensure that eligible Californians, especially people of color, keep their coverage and access the screenings, supports, and care necessary for their health and well-being.
Overall, Mayra Alvarez’s statement highlights the importance of health insurance coverage and access to care for marginalized children, particularly during the pandemic, and calls for addressing structural racism and administrative barriers to ensure continuous coverage for all eligible Californians.
The speaker discusses the importance of continuous coverage policy in stabilizing care and reducing coverage gaps for children. They highlight the issue of churn, which is the process of cycling on and off health insurance coverage, and how it can negatively impact children’s coverage. They provide data on the rate of churn prior to the federal health emergency and how it decreased during the public health emergency due to protections, resulting in 340,000 kids being protected from losing coverage.
The speaker emphasizes the need for families to update their contact information with their County to ensure they receive the medical renewal package and complete the necessary forms by the due date. They also call for an all-hands-on-deck effort, involving schools, childcare centers, churches, clinics, and community health centers, to spread the word about the importance of renewing medical coverage and ensuring that all eligible children and families can keep their benefits.
The speaker also highlights the upcoming expansion of medical coverage to undocumented communities in California, and the need to continue strengthening medical coverage for families, particularly for young kids aged zero to five. They express gratitude to leaders who prioritize the health and well-being of children and families and call for continued efforts to spread information and ensure the medical program remains strong for all eligible children and families.
Overall, the speaker delivers a clear and compelling message about the importance of continuous coverage and renewal of medical coverage for children and families in California, while acknowledging the challenges and the need for collaborative efforts to ensure that all eligible individuals can access and maintain their health insurance coverage.
#HealthCoverage #ChildrenAndFamilies #MediCal #LossOfCoverage #RenewalProcess #California #ContinuousCoveragePolicy #Churn #MedicalEnrollment #UndocumentedCommunities #MediCalExpansion #PolicyForContinuousCoverage #StrengtheningMediCal #HealthInsuranceCoverage #EligibilityForMediCal