Her journey from Cameroon, to the U.S. began with delivering babies. Now, she’s pioneering a movement to center science, dignity, and visibility in menopause care.
Magazine, Living Well, The Immigrant Experience
October carries a dual weight—and a shared opportunity. It is National Breast Cancer Awareness Month and World Menopause Awareness Month. While the former is spotlighted by global campaigns and pink ribbons, the latter remains quieter, tucked in the margins of medicine and media. Yet for millions of women, especially those in marginalized communities, breast cancer and menopause are intimately connected. Cancer treatments can trigger early menopause. Hormonal changes can raise cancer fears. And both journeys reveal how often women are misheard—or not heard at all.
This story honors both.
Dr. Fri Mofor Eta didn’t come to America to talk about menopause. She came to deliver babies. At twenty, she left Bambili, a small academic town in northwest Cameroon, carrying a dream shaped by faith, family, and a moment of awe watching a goat give birth outside her childhood window. That moment stirred a calling: to become a healer.
Years later, with a medical degree in hand and a career as a full-scope OB-GYN, Dr. Eta found herself in crisis—not in the delivery room, but on an airport floor, unable to walk, terrified she was dying. Test after test revealed nothing. Until finally, she faced the truth: this was perimenopause.
That moment cracked something open.
What began as a personal reckoning became a professional revolution. Today, as founder of Intentional Menopausing, Dr. Eta is leading a bold campaign to bring menopause out of hiding—through culturally grounded, science-informed, and soul-centered care. From Cameroon to the U.S., from birth to rebirth, her story is one of unlearning, awakening, and transforming midlife medicine for the women too often left behind.
She shares her story with Pamela Asobo Anchang, Managing Editor of The Immigrant Magazine, to illuminate a path forward for the millions of women suffering in silence.
Tell me about Bamenda and your early life in Cameroon. What dreams or beliefs did you carry with you to the U.S.?
 I grew up in Bambili, a small college town a few miles from Bamenda, in the 1970s and 80s. It was a time when everyone knew everyone, a close-knit, supportive community that felt like one big family. Later, I attended Our Lady of Lourdes Secondary School in Bamenda, a Catholic boarding school for girls, where I spent five unforgettable years. The friendships I formed there blossomed into lifelong sisterhoods that continue to this day.
I grew up in Bambili, a small college town a few miles from Bamenda, in the 1970s and 80s. It was a time when everyone knew everyone, a close-knit, supportive community that felt like one big family. Later, I attended Our Lady of Lourdes Secondary School in Bamenda, a Catholic boarding school for girls, where I spent five unforgettable years. The friendships I formed there blossomed into lifelong sisterhoods that continue to this day.
It was also at Lourdes that I learned a lesson that continues to shape my journey: success is not the result of one grand moment, but the sum of small, intentional efforts repeated every day. That belief has guided me throughout my life and continues to propel me toward every new height I reach.
At what moment did you first imagine you’d become a physician—an OB-GYN in particular?
I was ten years old when it happened. I was standing by the window, looking out at the small farm beside our house, when I heard a strange sound. Curious, I leaned closer and there she was, one of our pregnant goats, giving birth. I watched in awe as life entered the world right before my eyes. It was magical, almost sacred.
From that day on, I was hooked. I followed every pregnant goat, waiting for the moment they would deliver. I even helped once during a difficult birth. Something about it stirred something deep inside me, a calling. I couldn’t wait to grow up so I could help women bring life into the world. I didn’t just want it, I knew it. I’ve never wanted to be anything else.
What was your immigration journey like—leaving Cameroon at 20, navigating a new culture, and pursuing medicine in the U.S.?
I was twenty years old when I arrived in Houston TX USA, — wide-eyed, eager, and full of dreams of becoming an OB/GYN. Everything felt new, yet familiar. I was surrounded by Cameroonians and Nigerians at school and at work, so in many ways, it felt like home. I didn’t have to face the culture shock that many immigrants talk about, at least, not right away.
But then came the challenge I wasn’t prepared for the financial strain. It was heavy, and at times, it felt like my dream of going to medical school might slip away. Still, something inside me refused to give up.
How did your identity as an immigrant shape (or challenge) your early medical training and career?
The culture shock that hadn’t touched me in college finally arrived in medical school. I left Houston for Saba, in the Netherlands Antilles, and for the first time in my life, I was surrounded by people who weren’t African. It was unfamiliar, even intimidating, but my classmates were supportive. Together, we shared a common goal and worked tirelessly to achieve it, a lesson in the power of collaboration and perseverance.
Residency, however, tested me in ways I had never imagined. The environment was competitive, sometimes harsh, and filled with politics and backstabbing. As a shy, soft-spoken immigrant, I often felt out of place. Yet, those challenges became my greatest teachers. Over time, I learned to find my voice, navigate adversity, and carve my own path, emerging stronger, more resilient, and more determined than ever.
In your years as a full-scope OB-GYN, what were your biggest joys—and your biggest blind spots?
My greatest joy hands down has always been helping bring life into the world. There’s something truly miraculous about witnessing a new life enter the world — it never gets old, and it never stops filling me with awe. But shortly after finishing residency, I encountered a professional blind spot that surprised me: menopause care.
I quickly realized that women navigating the menopausal transition often face a significant gap in support and understanding. I had been completely unprepared and undereducated on just how deeply menopause can impact every aspect of a woman’s life — physically, emotionally, and socially. It was a humbling moment, but it also became a turning point, igniting a new passion to help women not just at the start of life, but throughout every stage of it.
 When did your own menopause symptoms begin, and how did you initially respond to them?
When did your own menopause symptoms begin, and how did you initially respond to them?
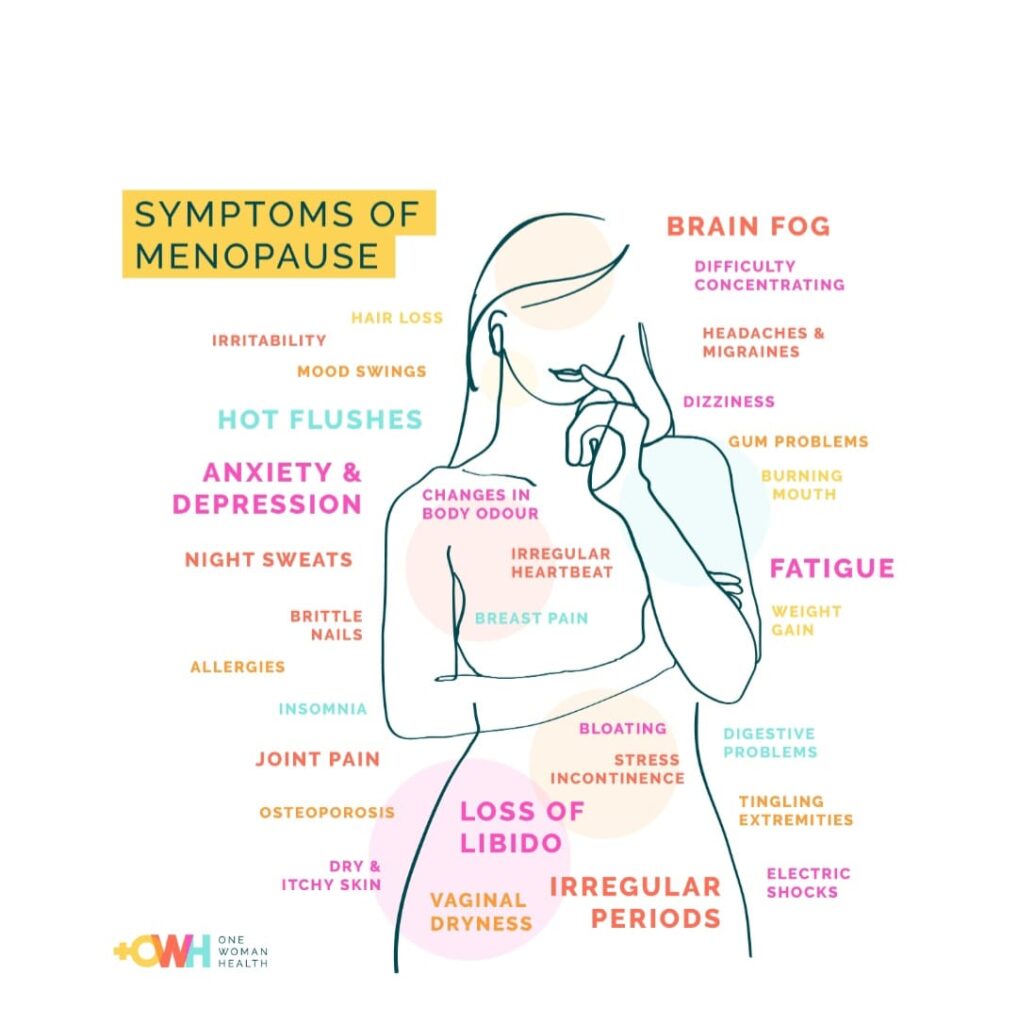
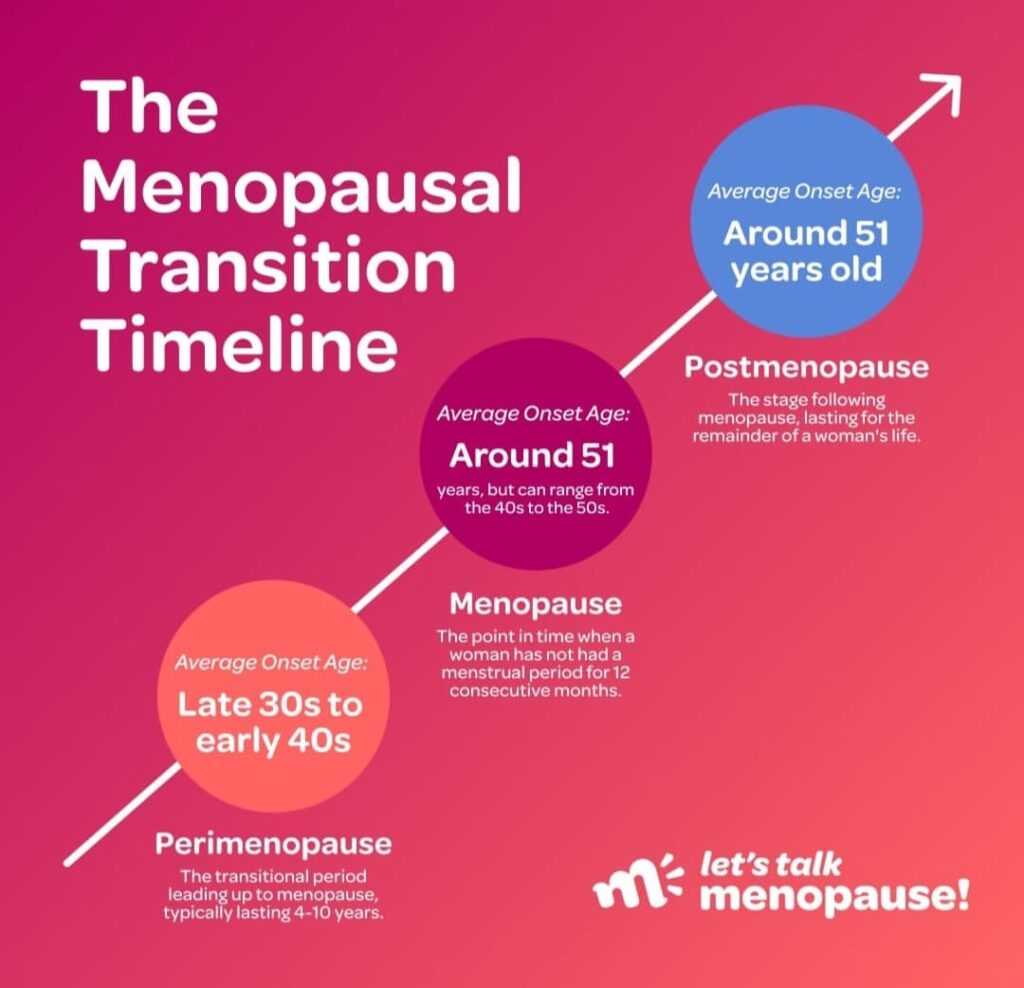
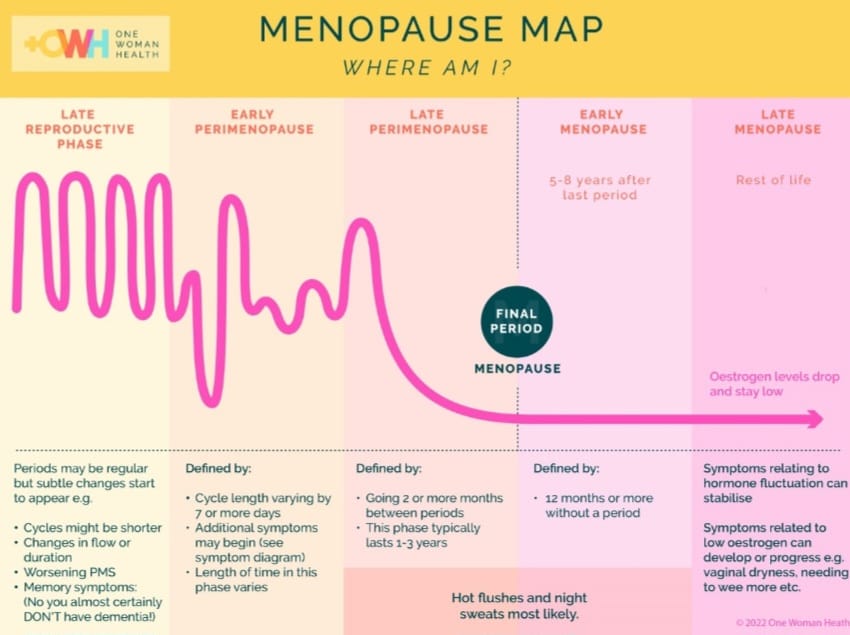
It’s well known that menopause is often a retroactive diagnosis, and I believe the same is true for perimenopause. Looking back, I realize that the symptoms I’ve been experiencing for more than five years, body aches, brain fog, and more, were most likely related to this transition. For years, I didn’t connect them to hormonal changes, in part because no one was talking about these symptoms, and lectures on perimenopause were nonexistent.
I also carried a misconception ingrained in me from medical school: the idea that women tend to somaticize psychological problems. So, naturally, I gaslighted myself, telling myself my symptoms weren’t as serious as they felt. When they persisted, I doubled down, refining my diet, increasing exercise, and trying nearly every nootropic I could find. Like many perimenopausal symptoms, these issues would wax and wane, but for about a year, they became constant and more severe. That’s when I realized something was truly wrong with my body and decided it was time to seek help.
What was the turning point that made you realize: “This is perimenopause”?
As I mentioned earlier, one of the biases we unconsciously learn in medical school is that women tend to somaticize psychological problems. I internalized that belief, and for years, whenever a woman came to me with a long list of vague physical symptoms, I would quietly assume it was “all in her head.”
So when I became that woman, with my own growing list of unexplained symptoms, I did the same thing to myself. I gaslighted my own experience, telling myself it was stress, burnout, or exhaustion.
Then one day, after a three-hour flight, everything came to a head. Severe pain, numbness, and tingling struck my left leg, leaving me barely able to walk. I lay down on the airport floor, propped my leg against the wall, and watched people walk past me walking easily, while I couldn’t. I massaged my leg, took Tylenol, calcium, magnesium, potassium, nothing helped.
And then the palpitations hit. My heart raced like never before, and my mind spiraled to the worst possibilities: ALS, MS, heart failure. I was convinced I was dying. An older woman approached me gently and asked, “Are you alright?” I choked back tears and whispered, “I don’t know.” Her kindness steadied me, and about an hour later, I managed to drag my leg to my car.
That moment was a wake-up call. In the days that followed, I dove into research and scheduled appointments with neurology, rheumatology, and cardiology. At one point, I came across a research paper by Dr. Vonda Wright on the musculoskeletal syndrome of menopause, then another NIH paper on palpitations during menopause.
I was stunned. How could I, an OB/GYN, be so undereducated on something that affects every woman, including myself? How could I have missed my own diagnosis? Still, I found it hard to believe that menopause, something we were taught to view as a natural, almost benign transition could cause symptoms this severe.
But after countless appointments and perfectly normal test results, I had no choice but to face the truth: my symptoms were due to perimenopause. That realization changed everything. It deepened my understanding of the challenges women face during this transition and ignited a new passion to bridge this gap in care, to advocate for women’s health, and to ensure that no woman feels dismissed or unseen the way I once did.
How did that experience reshape your medical philosophy and lead you to retrain yourself as a menopause expert?
It changed everything.
First of all, I believe women when they tell me something is wrong. For far too long, women have been conditioned to endure unimaginable pain and discomfort in silence and when they finally speak up, they’re often told it’s all in their heads. I know now, firsthand, that it’s not.
Secondly, this experience opened my eyes to a major gap in our healthcare system: most physicians are not adequately educated about the menopausal transition. When women present with symptoms like brain fog, joint pain, fatigue, or mood changes, these are rarely recognized as possible signs of perimenopause. Instead, they’re often labeled with diagnoses such as fibromyalgia, arthritis, anxiety, or chronic fatigue syndrome.
Even within my own specialty, OB/GYNs tend to associate menopause primarily with hot flashes, irregular periods, and insomnia. This narrow view leaves a significant gap, a missing link to connect the wide spectrum of symptoms women experience during this transition.
That’s where menopause providers like myself come in. We bridge that gap. We listen. We validate. And we guide women through this transformative stage of life with compassion, understanding, and science-backed care.
Why did you create Intentional Menopausing, and what does it mean to “menopause intentionally”?
I created this platform because of the enormous gap in menopause care that I’ve witnessed both personally and professionally. I realized there was a deep need for a space where women can speak up and truly be heard, understood, and validated.
A space where they can learn what’s happening in their bodies, why it’s happening, and what they can do to improve their experience of the menopause transition. A space where we can debunk myths, shatter stigmas, and redefine what this stage of life means for women everywhere.
My mission is to empower women with knowledge and science-backed tools they can use to make intentional choices — choices that not only enhance the quality of their lives today, but also help prevent chronic, disabling diseases in the years to come.
I chose the name “Menopausing” because here, we act consciously and intentionally. We leave nothing to chance. I believe that a great life isn’t stumbled upon; it’s built, one conscious, science-informed, and purposeful actionable choice at a time.
Who are you hoping to reach most with this work—and why now?
Everyone! But especially the women in the thick of it.
Menopause affects more than just the woman going through it. Partners, children, friends, and co-workers are all impacted, and each of them can benefit from understanding this transition better.
Younger women who haven’t reached this stage yet can also learn how to care for their bodies now, so they can move through menopause with greater ease when the time comes.
And for the women who see themselves in me, those who connect with my story, my race, or my culture, I want you to know that your experiences will be heard, understood, and validated here.
My goal is to reach everyone, so that together, we can shatter the taboo around menopause and bring this long-overdue conversation into the mainstream.
What are the most harmful myths or gaps you see in how menopause is treated, both medically and culturally
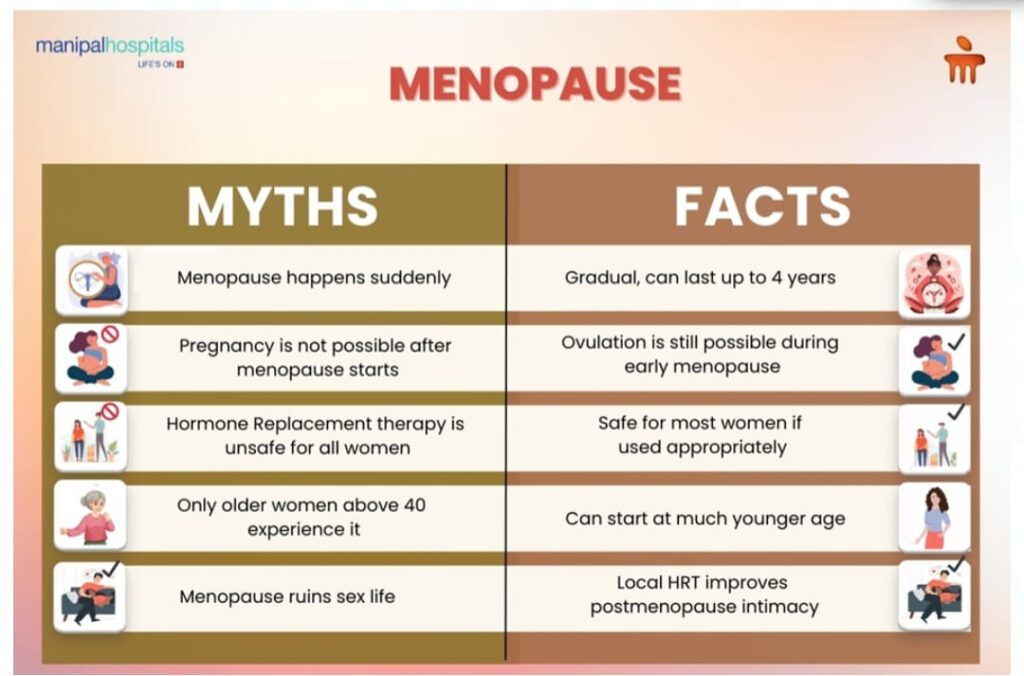
This fear started back in 2002 after a big study, the Women’s Health Initiative, made headlines saying hormone therapy increased breast cancer, heart attacks, and strokes. That news spread fast and scared both women and doctors.
But here’s what we now know: those results were misinterpreted. When the data was reanalyzed, the increased risks turned out to be not statistically significant. In fact, when used correctly, estrogen actually protects the heart, brain, bones, and even the breasts.
The women in that study were older and less healthy than the women who typically start hormone therapy today. They also received much higher doses and the hormones used were synthetic, not the body-identical ones we use now.
So the truth is, the findings from that old study don’t apply to modern menopause care. Unfortunately, the fear it created still lingers and it’s stopping too many women from getting the safe, effective, and life-changing care they truly deserve.
The second big myth I hear all the time is that taking herbal supplements is somehow more “natural” or safer than hormone therapy.
Here’s the truth, the hormones we use today in HRT are body-identical, meaning they have the exact same chemical structure as the hormones your body naturally makes, the same ones it’s now craving during perimenopause and menopause. These hormones bind to specific receptors in your body and support essential metabolic functions in the brain health, heart, muscles, bone and every other organ system in your body.
On the other hand, most herbal or plant-based supplements are foreign to your body. Your body doesn’t have natural receptors for them, so while they may offer mild benefits for some people, they can’t actually restore your body’s hormonal balance or bring you back to homeostasis.
So “natural” doesn’t always mean better. Sometimes, science-backed and body-identical is the most natural choice.
How do race, immigration, or cultural background impact how women experience or talk about menopause?
The menopausal transition is a biopsychosocial experience, meaning it affects not only a woman biologically, but also impacts her psychological well-being and social life. Differences in these aspects across races and cultures lead to a wide range of experiences. Cultural beliefs, societal views of aging, and communication norms shape whether women perceive menopause as a problem, a natural transition, or a rite of passage and whether they feel comfortable discussing it. Race and immigration can also influence symptom patterns, stress levels, and access to culturally sensitive healthcare, creating varied experiences for different women. In the 1990s, a longitudinal research study, The study of Women’s health Across the Nation (SWAN) was started, and has shown for example that, black women may experience menopause about a year earlier than non-black women and have earlier, more severe hot flashes and a longer duration of perimenopause. I should note that more severe hot flashes are a risk factor for cardiovascular disease and diabetes. Women of color also frequently face medical bias, which can further limit open discussion of symptoms thus limiting the care their care.
What support or resources does Intentional Menopausing offer that you wish had existed when you were in transition?
Data! Science-backed knowledge is everything. It’s the data from rigorous scientific studies — the kind that tells us exactly what works, what doesn’t, and why. It gives us concrete information so we don’t have to waste time on trial and error. Luckily for me, I’m still navigating this transition myself, and applying this data has made a tremendous difference in my life now and for the years to come.
Also, we are in the process of setting up our telehealth services to improve access to hormonal and non-hormonal options for treatment for menopausal symptoms.
Can you share a patient story or success moment that affirms why this work matters?
Ms. J is 49 years old and had been struggling for years with perimenopause symptoms, weight gain, brain fog, insomnia, low libido, painful intercourse, musculoskeletal aches, and fatigue. Like many women, she had fallen prey to the myth that HRT was bad and thus avoided it. By the time she came to me, nothing she had tried was working, and she had very little energy for daily activities.
Her symptoms indicated deficiencies in estrogen, progesterone, and testosterone. We developed a tailored plan to “stack” her hormones, introducing them one at a time over 4 to 6 months. Estrogen was started first, both systemic and vaginal and by the second month, her energy returned. She was back in the gym, losing fat and building muscle. She eats an anti-inflammatory diet, sleeps better, has a passionate, pain-free sex life, says she feels like herself again and is living the life of her dream. Results like this make what I do worth it!
What’s one piece of advice you’d give to any woman entering midlife unsure of what’s happening in her body?
My advice is to trust your body and give yourself permission to ask questions. The menopausal transition is a wake-up call, a signal that our bodies are speaking to us and need attention to function at their best.
Even though many symptoms during this transition aren’t signs of current disease, they can be risk factors for future health issues. For example, hot flashes may indicate higher cardiovascular risk, and brain fog could signal an increased risk for possible dementia.
In that sense, these symptoms are actually a gift. They give us a glimpse of what the future might hold and, more importantly, an opportunity to make conscious, informed choices today to protect our health tomorrow.
Looking ahead, what’s your vision for menopause care in the next 5–10 years?
In 5 to 10 years, my vision is to help transform how the world understands and supports women as they traverse the menopausal transition. I see a future where menopause is no longer whispered about or dismissed, but openly discussed, celebrated, and supported with the same attention and innovation as any other stage of life. I envision a world where every provider will have ample knowledge of the menopausal transition and where all the myths about menopause and it’s treatments will be debunked. Through this platform and many others, I see millions of women empowered with science backed knowledge and tools they can use to take control of their health, live with vitality, avoid debilitating and immobilizing diseases and thus change the trajectory of their lives.
Lightning Round
A book every clinician should read?
The New Menopause by Dr Mary Claire Haver. Because I believe it will go a long way in closing the gap of knowledge clinicians have when it comes to menopause care.
A daily self-care ritual you swear by?
Resistance training. Because the skeletal muscle is the organ of longevity, a true metabolic power house that if maintained will be the organ that preserves our function, our independence, prevent many chronic diseases and also reduce all cause mortality.
A menopause myth you’d erase forever?
The biggest myth is that HRT is bad.
We now know that’s simply not true. Modern hormone therapy not only relieves the symptoms of perimenopause and menopause, but it also helps prevent a range of chronic diseases. Research shows that women who use HRT appropriately live longer and healthier lives than those who don’t.
A woman who inspires you?
Oprah Winfrey!
From humble beginnings, she carved her own path and never let failure define her. She lives life on her own terms, authentically, courageously, and with purpose. It’s easy to see that she’s guided by her soul, and that’s what makes her truly inspirational to me.
Dr. Fri Mofor Eta’s story is not just about healing—it’s about reclaiming. Reclaiming the narratives women have lost to silence. Reclaiming the science dismissed by fear. Reclaiming midlife not as a slow descent, but as a portal to strength, strategy, and self-knowing.
As an African OB-GYN, as an immigrant woman, and as a midlife trailblazer, Dr. Eta is living proof that medicine can be both technical and tender. Through Intentional Menopausing, she’s building a future where women are not only treated—but understood. Where no woman is told “it’s all in your head.” Where hormonal shifts are honored as signals, not shame.
In her hands, menopause is not the end of a story—it’s the rewriting of one. One choice, one voice, one woman at a time.
To learn more or connect with Dr. Fri Mofor Eta’s work, visit her platform Intentional Menopausing on Facebook—where education, empathy, and community come together to support women through the midlife transition and beyond.
#IntentionalMenopausing #MidlifePower #ImmigrantVoices #MenopauseAwareness #AfricanDoctors #BlackWomenHealth #WomensHealthMatters #HormoneTherapy #PerimenopauseSupport #HealthEquity
Stay proud. Stay grounded. Stay true.


